Velocity Medical Billing is a trusted Medical Coding Help Company, offering expert consulting services specifically designed for your coding needs. Our skilled coding consultants work closely with healthcare providers to ensure your coding processes are accurate and compliant. By deeply integrating with your practice, we identify opportunities to minimize errors and streamline coding workflows.
Our consulting team provides the strategic guidance and tactical support needed to optimize your coding processes, technology, and staff proficiency. With our consultancy solutions, every practice is positioned to thrive through enhanced medical coding accuracy and efficiency.
Velocity Medical Billing optimizes the entire credentialing process to ensure accurate provider data entry, expedite credentialing approvals, and enhance reimbursement rates. The result? Faster approvals, reduced errors, and more satisfied providers.
Velocity Medical Billing collaborates closely with healthcare facilities to ensure accurate and timely credentialing of providers. By streamlining the credentialing process and ensuring quick approvals, we help facilities enhance their revenue and support sustained growth.
As a specialized medical credentialing consultancy, Velocity Medical Billing offers strategic advisory services to enhance your practice's operational efficiency. Our experts identify and resolve credentialing issues that cause delays and implement streamlined processes to ensure quicker approvals and smoother onboarding.

As a leading medical credentialing consulting company, Velocity Medical Billing provides specialized experts for each specialty’s credentialing workflows. Our team is dedicated to streamlining the credentialing process through comprehensive management of provider data, thorough documentation, and efficient follow-up procedures. By applying our extensive knowledge of credentialing requirements and regulations, we ensure that healthcare providers achieve timely and accurate credentialing.
We assist practices of all sizes in overcoming challenges related to credentialing delays, lost applications, and other issues. Our 24/7 credentialing consultancy offers expert support to ensure that every provider is credentialed promptly, allowing your practice to focus on delivering excellent patient care while we handle the complexities of credentialing.
Our credentialing teams are more than just experts. We are every USA provider’s premier credentialing partner. Our medical credentialing specialists work closely with healthcare providers to enhance practice management and drive sustainable growth. Here’s how Velocity Medical Billing supports practices with efficient and effective credentialing:


Credentialing can be prone to errors, delays, and inefficiencies that impact your practice’s operational efficiency and revenue. Velocity Medical Billing’s credentialing specialists streamline your clinic’s credentialing process by managing the entire credentialing cycle with real-time updates and detailed analytics.
Gain insights into crucial performance indicators, including copays collected and accounts receivable by payer, to effectively monitor and manage your practice’s financial health.
Monitor your practice’s revenue by tracking patient and insurance payments, identifying trends, and assessing financial progress to ensure effective management and growth.
Send reminder notices to patients with overdue payments and collect outstanding balances to minimize receivables and improve cash flow.
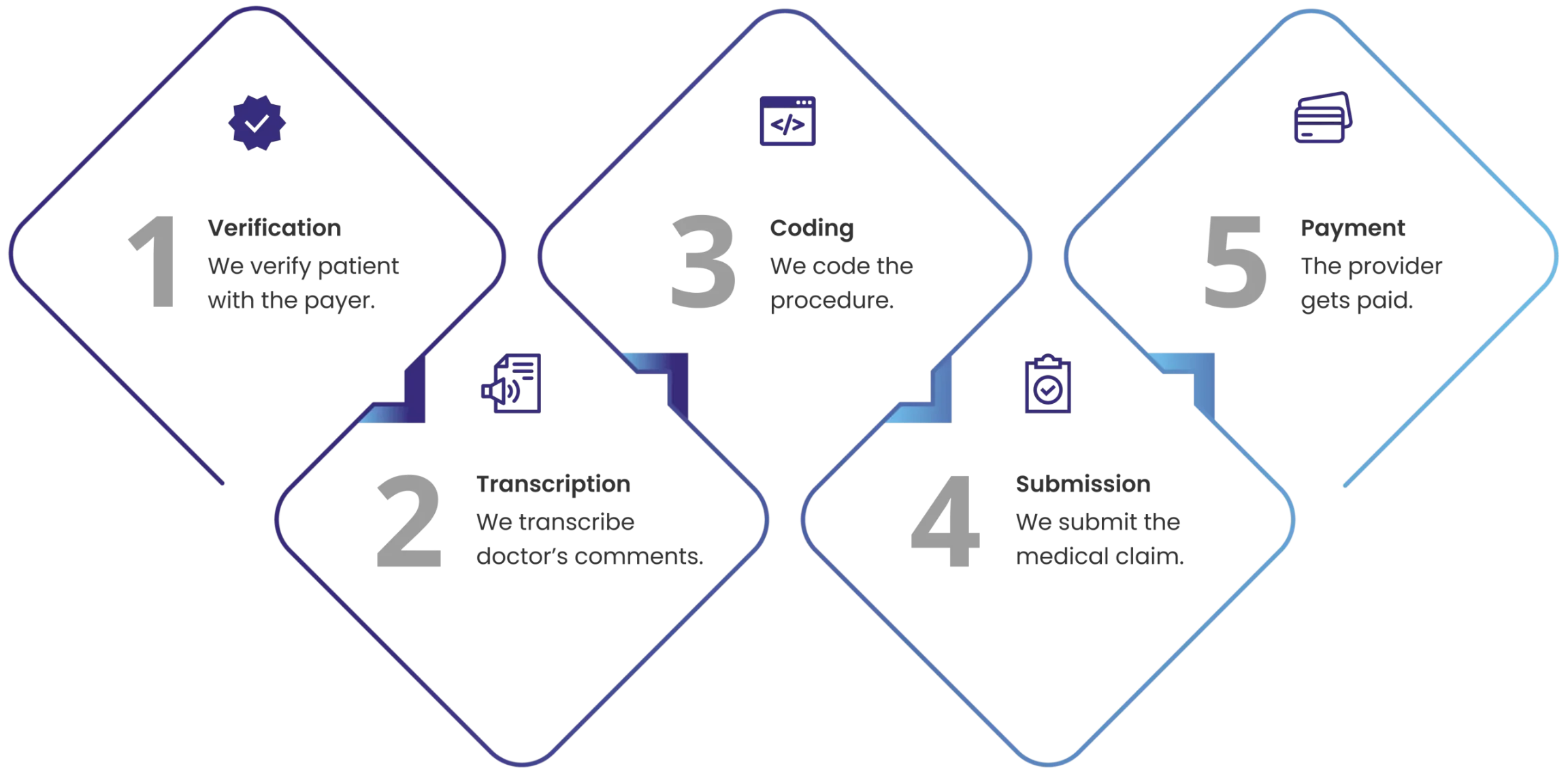
The system verifies a patient’s insurance benefits at check-in to prevent billing surprises and prompts patients to pay co-pays at this time.
Get a swift overview of your practice’s financial performance and develop targeted initiatives to enhance and scale your practice effectively.
Obtain a comprehensive summary of your medical bills, including their status (paid, denied, in process, rejected). Our experts will follow up on these bills and offer one-click support for resolving any billing issues.
Our AI-powered billing rules engine automatically detects and corrects errors in medical claims, ensuring faster payments and higher reimbursement rates.
Smart billing with precise charge coding ensures accurate and compliant superbills, eliminating the risk of upcoding or downcoding.
AI-powered algorithms recommend the appropriate E&M level and detect and prevent medical fraud, eliminating the need for a separate coder.
Physicians can greatly benefit from our medical credentialing consultation services. Our expert credentialing consultancy enhances accuracy, speeds up provider approvals, and improves practice efficiency. We achieve this by customizing our services for each practice and addressing specific challenges with tailored solutions.